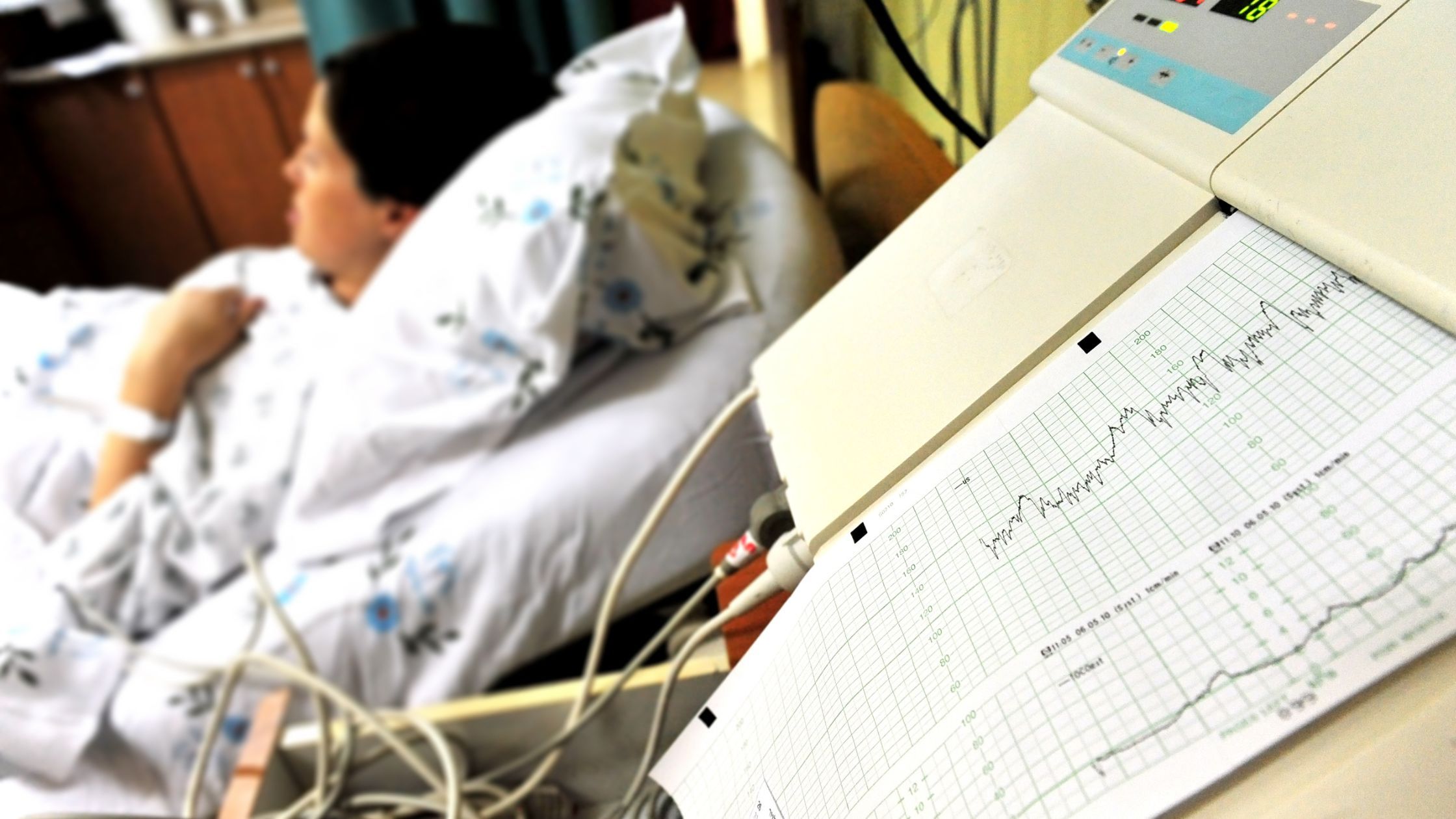
Importance of fetal monitoring during labour
Fetal monitoring is an important means of identifying fetal distress. Approximately one in four labours or births are complicated by fetal distress (HSCIC 2015)
There are two main methods of monitoring the fetus:
- Intermittently.
- Continuously, also called continuous electronic fetal monitoring (“EFM”) and sometimes shortened to cardiotocography (“CTG”).
Intermittent monitoring
Listening to the fetal heart rate using a stethoscope may be appropriate for a healthy woman in labour who has experienced an uncomplicated pregnancy. This should involve documenting the heart rate for a minimum of 60 seconds at least:
- Every 15 minutes including after a contraction in the first stage of labour.
- Every 5 minutes including after a contraction in the second stage of labour.
Monitoring may need to be continuous if the abovementioned monitoring is abnormal or if any risk factors develop during labour.
How is the fetus monitored during labour
The CTG is used to monitor the fetus during labour. The CTG is an electronic fetal heart rate monitoring used to evaluate fetal wellbeing both antenatally and during labour.
In addition to the fetal heartrate, uterine activity should also be recorded.
There are four features of the CTG which should be assessed individually and subsequently, taken together with the clinical picture to decide the appropriate management required. The four features are:-
- Baseline fetal heart rate. This is the mean level of fetal heart rate over a period of 5 to 10 minutes. The normal range is 110 – 160 beats per minute (“BPM”). In pre-term fetus’, the baseline is ordinarily at the higher end of this range.
- Baseline variability. This accounts for minor fluctuations that take place in the baseline fetal heart rate at 3 to 5 cycles per minute.
- Accelerations in the fetal heart rate of 15BPM or more lasting for 15 seconds or more.
- Decelerations in the fetal heart rate of more than 15BPM lasting 15 seconds or more.
What do CTG results mean?
The results of the CTG can be considered as either normal, suspicious or pathological (two or more features are non-reassuring, one is abnormal).
The purpose of monitoring the fetus during labour is to detect potential complications at an early stage and treat or act on such complications before experiencing significant consequences. The main reason is to detect fetal hypoxia (low oxygen levels of the fetus) and thus prevent acidaemia and cell damage.
Complications potentially identified if monitored correctly
- Uterine hyperstimulation
- Umbilical cord compression
- Placental abruption
- Sudden maternal hypotension
- Meconium in the amniotic fluid, and the fetus has inhaled it. This may cause infection to the fetus or block the fetus’ airways.
Some complications, if left untreated, may escalate to fetal hypoxia.
Chronic fetal hypoxia may result in myocardial damage (heart damage). The consequences may be lifelong and devastating.
Examination of mother if abnormal CTG
If the CTG is abnormal, examination of the mother should be conducted to help determine the cause of the increase fetal heart rate and/or abnormal uterine activity.
Mother’s temperature
The mother’s temperature should be assessed. A raised temperature may provide explanation for the increase fetal heart rate, such as ruptured membranes for a period of more than 24 hours, thus increasing the risk of infection.
Mother’s pulse
If the fetal heart rate has decreased, investigations should be made to ensure the treating clinician has not recorded the heart rate of the mother.
Mother’s blood pressure
If the mother has experienced hypotension and has thus been treated with epidural anaesthesia, this may reduce the blood flow to the uterus and cause the fetal heart rate to decrease. Treatment should be administered, and mother’s blood pressure regularly checked to identify and treat this.
Abdominal examination of the mother
The size of the abdomen should be assessed to determine if this is consistent with the dating of the fetus.
Vaginal examination
This should seek to assess the dilation of the cervix in order to determine the progress in labour but to also ensure the fetal cord is not present. The presence of a fetal cord may suggest cord prolapse. This can be associated with the fetal heart rate decreasing. This is an emergency situation mandating immediate delivery by caesarean section if the cervix is not fully dilated.
What should happen if the CTG is abnormal
If the CTG is deemed suspicious, as discussed above, it may be decided to treat the woman conservatively. This may involve changing maternal position.
However, if the CTG is pathological, fetal blood sampling should be performed. The results may indicate that immediate delivery is required or that the test needs to be repeated in either 30 or 60 minutes’ time (depending on the results).
However, if fetal blood sampling is not possible, for instance if there are inappropriate facilities, delivery should be expedited by caesarean section.
Negligence may occur when:
- Fetal Heart rate has not been adequately monitored during labour.
- Monitoring of the fetal heart rate has now been increased following abnormal results or any risk factors developing.
- Mother has not been assessed or examined correctly following abnormal results.
- Urgent action hasn’t been taken when required as indicated by fetal heart rate monitoring.
- Failure to appropriately interpret results following monitoring of fetal heart rate.
The complications as outlined above can be lifelong and devastating. There are occasions when the complications are unavoidable but there are instances when such complications are the result of avoidable negligence, and thus may have been prevented if appropriate treatment was provided.
If you are concerned that you or a loved one has experienced negligence, please do contact us and ask to speak with a specialist solicitor within our clinical negligence team. Please note, the information contained herein is not to be treated as medical or legal advice. Please revert to your treating clinician or obtain solicitor advice for further information.